Preparing for Conception: Naturopathic Perspectives
Thinking of conceiving? You may have heard about the “100 days”—the time it takes for an egg to mature. For men, it takes about 80 days for sperm to mature. During this time of development and maturation, a woman’s follicles and a man’s sperm are extremely vulnerable to DNA damage from exposure to toxins, systemic or chronic inflammation, and nutrient deficiencies. This means that for many who are ready to or are thinking of conceiving in the not-so-far future, the health of their eggs and sperm can be greatly impacted before they are even released, either during ovulation or ejaculation. This is the window that we need to take advantage of, to increase the health of our eggs and sperm to increase the odds of a viable and healthy egg and fertilization.
Although we place a lot of importance on women for fertility, sperm health, measured by proper morphology (shape) and motility (the ability to move and swim properly), directly relates to male health. If sperm are dysfunctional, if there are fragments in DNA or abnormal head or tail shapes, there’s a small likelihood that sperm is going to make it to the egg, let alone fertilize it.
Planning for a healthy pregnancy therefore actually starts before conception and needs to include both partners. The health of a mother who nourishes a fetus is critical, but so is the health of the partner whose sperm—and therefore DNA—will be incorporated into making an embryo.
The point isn’t to scare couples but to empower them. There are many things that you can do for your health that will affect that of your eggs and sperm.
Take a High-Quality Prenatal Vitamin and Vitamin D
Multiple nutrients and vitamins are essential for reproductive health, including several B vitamins, vitamin D, and folic acid. Speak to your naturopathic doctor for recommendations. Not all prenatal multivitamins are made equally. There are many products available that contain cheaper, synthetic forms of vitamins, as well as formulas that include multiple fillers and artificial food dyes. Most importantly is getting 1 mg of folic acid, which we find is optimal in the methylated or naturally occurring form, 5-methyltetrahydrofolate (5-MTHF).[1]
5-MTHF has its advantages over “plain old” folic acid. It’s better absorbed in the gastrointestinal tract and is bioavailable, even in a person with genetic SNPs or “snips” for the folic acid enzyme MTHFR. Additionally, using this form reduces the risk of masking the symptoms of a B12 deficiency, making it a superior form of folic acid.[1]
Vitamin D is a major modulator of steroidal sex hormones. Now, in winter, most of us in North America are deficient in vitamin D. Having optimal levels can lead to better odds of embryo implantation and clinical pregnancy. This is especially important in endometriosis and any women who has experienced recurring pregnancy loss.[2]
 Understand Your Cycles and Track Your Ovulation
Understand Your Cycles and Track Your Ovulation
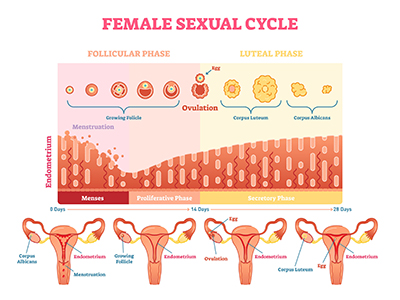
Using tools like fertility awareness methods can help identify your fertile window. While textbooks say that a women should ovulate on day 14 of her cycle, many women actually ovulate sooner or later than that. Therefore, if you’re only engaging in intercourse around day 14, you might be completely missing your fertile window.
Be mindful and track your cervical fluid and discharge quality. It can also be helpful to track your basal body temperature each morning to find out when you’re ovulating.
Eat Organic When Possible, and Eat a Variety of Fruits and Vegetables
Nutrition is key! Consuming nutrients via a healthy diet and a prenatal vitamin plays a significant role in overall health. The focus should be on including more vegetables and one or two servings of fruit per day. Whole, complex carbohydrates are also important for hormone regulation and digestion (elimination).
High-quality protein and healthy-fat consumption is also essential. Fast food, fried foods, refined sugars, and sweeteners such as corn syrup should be avoided. The goal is to protect your reproductive cells while providing the building blocks and cofactors the body needs to run properly and efficiently. We can influence this by promoting anti-inflammatory pathways and in providing antioxidants to scavenge the free radicals that can cause DNA fragmentation.
Remember: You’re going to want to nourish your body with proper nutrition during pregnancy anyway, so why not start now?
 Avoid Alcohol
Avoid Alcohol
One study showed that women consuming 25 g of alcohol (about one 8 oz glass of wine) daily had a decrease in embryo quality. 70% of the embryos analyzed from women consuming alcoholic beverages regularly showed deviations in the degree of DNA fragmentation (10–25%), symmetry, and division pace.[3]
Of the embryos analyzed, only 15% of those from women who consumed alcohol were classified as “class A” embryos, meaning they had the highest reproductive potential. By comparison, in those women who did not consume alcohol, 42% of the embryos were identified as “class A.”[3]
Alcohol consumption can negatively impact male reproduction as well. Alcohol has been shown to affect sperm morphology and motility (their shape and ability to move) and can lead to low testosterone levels.[4]
Limiting or eliminating alcohol consumption may lead to the production of higher-quality embryos and may increase the odds of success when using advanced reproductive techniques (ART) such as in vitro fertilization (IVF).[3]
Avoid Exposure to Household and Environmental Toxins, and Improve Your Body’s Ability to Detoxify and Eliminate Waste
Detoxification pathways in the liver are metabolically demanding. This means that nutrients from diet and supplements are used in multiple reactions in our cells. One report from a study called “Toxic Nation: A report on pollution in Canadians” revealed that human volunteers had measurable levels of 41 different carcinogens, 27 hormone disruptors, 21 respiratory toxins, and 52 reproductive and developmental toxins.[5] This included organophosphate insecticides, organochlorine pesticides, and volatile organic compounds (VOCs).
We know that we have daily exposure to these substances. For the most part, our bodies can detoxify and excrete many of them, often either through urine, stool, and/or sweat.
In ensuring proper detoxification, we must manage three different major aspects:
- Reduce exposure to toxins: Microwaving food in plastic containers, BPAs (which can also be found in the lining of canned food), fragrances/parfum and parabens (found in beauty and body care products), car exhaust fumes, cigarette smoke, air fresheners, and even many household cleaning products.
- Obtain adequate nutrition and take vitamins and mineral supplements as prescribed. These compounds are our cofactors for detoxification pathways.
- Maintain regular elimination: Drink about 2 litres of water per day, and urinate. I’ve had many patients claim they don’t drink enough water because it’s inconvenient to visit the bathroom so often. Go to the toilet! Your body is supposed to filter and eliminate. While you’re thinking about it, make sure you’re having regular, daily bowel movements.
 Get Adequate Sleep and Manage Stress
Get Adequate Sleep and Manage Stress
At least 7.5 hours per night are required for overall health. Stress management also plays a role in this, for many people are “tired but wired” or feeling restless in the evening or before bed. Sleep and stress management will help promote repair mechanisms in the body, restoring body and brain tissue, regulating your body temperature, and inducing key genes to turn on and off for optimal health. Stress can also negatively impact our sex hormones, leading to lower levels of progesterone, estrogen, and luteinizing hormone as well as to higher odds of anovulation (not ovulating in a menstrual cycle).[6]
 Exercise or Participate in Some Form of Regular Physical Activity, and Work to Obtain Your Healthiest Body Composition
Exercise or Participate in Some Form of Regular Physical Activity, and Work to Obtain Your Healthiest Body Composition
By following the recommendations above, consuming adequate amounts of protein daily and engaging in regular physical activity, you may already find yourself with a healthy body composition. Ideally, women want to have between about 18–25% body fat.[7] Outside of those ranges, we commonly see hormonal disorders such as anovulation, irregular periods, amenorrhea, and other sequelae such as miscarriage.[8]
Pregnancy can be taxing on a woman’s body physically. In addition to nourishing and housing her growing fetus, her body then must give birth, when the structures within the pelvis undergo dramatic changes. Strengthening the body is an important aspect of preparing for conception, but also for pregnancy and labour.
Strength-training is a great way to build muscle; however, even just going for a daily brisk walk for 20–30 minutes will greatly help circulation while elevating the heart rate to help improve endurance.
Yoga can be incorporated for strengthening and improving posture, but also for practicing physical exertion while focusing on the breath. Being able to breathe through physical discomfort and muscle contractions is a great tool for practicing how to cope with the demands of labour. As a bonus, yoga is great for helping reduce feelings of stress!
For those who are not physically fit or are just getting into an exercise regimen, it’s best to start off slow and focus on proper body mechanics. For at-home workouts, have a mirror in the room so you can watch your form. Most gyms and yoga studios include floor-length mirrors in the space so that you can watch your alignment and movements. Beginners and those with past injuries should consult with a doctor or physiotherapist before starting any new workout program.
Ask Your Partner to Join You on Your Preconception Health Journey
Both partners play major roles in a couple’s fertility. Sperm are vulnerable to DNA damage, just as a women’s oocytes are. Sperm also need proper nutrients such as selenium and zinc for proper development and motility. Going through these healthy changes together is also a wonderful way to bond and to feel good about your health together. Go for walks with your partner, cook together, and support each other mentally and emotionally through this exciting stage in your lives.
References
- Scaglione, F., and G. Panzavolta. “Folate, folic acid and 5-methyltetrahydrofolate are not the same thing.” Xenobiotica, Vol. 44, No. 5 (2014): 480–488.
- Lerchbaum, E., and B. Obermayer-Pietsch. “Vitamin D and fertility: A systematic review.” European Journal of Endocrinology, Vol. 166, No. 5 (2012): 765–778.
- Wdowiak, A., et al. “Alcohol consumption and quality of embryos obtained in programmes of in vitro fertilization.” Annals of Agricultural and Environmental Medicine, Vol. 21, No. 2, (2014): 450–453.
- La Vignera, S., et al. “Does alcohol have any effect on male reproductive function? A review of literature.” Asian Journal of Andrology, Vol. 15, No. 2, (2013): 221–225.
- Neumann, J., et al. Toxic nation: A report on pollution in Canadians. Toronto, Environmental Defence, 2015, 48 p., ISBN 0-9737195-1-6. · Available at https://d36rd3gki5z3d3.cloudfront.net/wp-content/uploads/2016/01/Rev_English-Web-Toxic-Nation.pdf · Retrieved 2018-02.
- Schliep, K.C., et al. “Perceived stress, reproductive hormones, and ovulatory function: A prospective cohort study.” Epidemiology, Vol. 26, No. 2, (2015): 177–184.
- Sharma, R., et al. “Lifestyle factors and reproductive health: Taking control of your fertility.” Reproductive biology and endocrinology, Vol. 11 (2013): 66.
- Jungheim, E.S., J.L. Travieso, and M.M. Hopeman. “Weighing the impact of obesity on female reproductive function and fertility.” Nutrition Reviews, Vol. 71 Suppl. 1 (2013): S3–8.
- - -
 Sarah Zadek, ND, is a licensed naturopathic doctor in Ontario, graduating from the Canadian College of Naturopathic Medicine in Toronto.
Sarah Zadek, ND, is a licensed naturopathic doctor in Ontario, graduating from the Canadian College of Naturopathic Medicine in Toronto.

 Stores
Stores